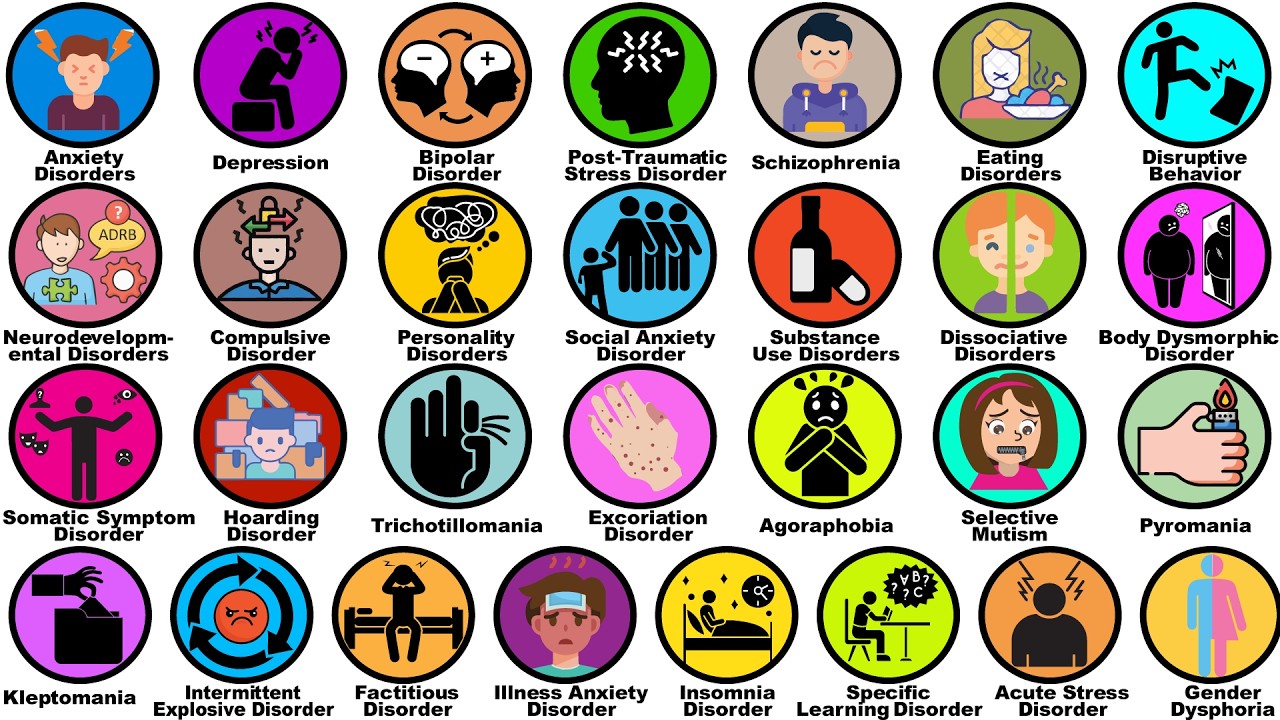
‘A massive global genetics study is reshaping how we understand mental illness—and why diagnoses so often pile up. By analyzing genetic data from more than six million people, researchers uncovered deep genetic connections across 14 psychiatric conditions, showing that many disorders share common biological roots. Instead of existing in isolation, these conditions fall into five overlapping families, helping explain why depression, anxiety, PTSD, bipolar disorder, schizophrenia, and substance use disorders so frequently occur together.…’ (via ScienceDaily)
Findings such as these resonate strongly with the stance of diagnostic skepticism that I have held throughout my career as a clinical and academic psychiatrist. Psychiatry has repeatedly taught us that its categories are provisional tools rather than natural kinds, and that our confidence in them often outpaces the solidity of the underlying science. The recurrent experience of patients accumulating diagnoses over time—sometimes within a single hospitalization, sometimes across decades—has always suggested that something more fundamental than discrete disease entities is at work.
Historically, this tension is not new. Psychiatric classification has oscillated for more than a century between lumping and splitting. At certain moments, the field has favored broad, integrative constructs—neurosis, psychosis, affective illness—emphasizing shared phenomenology and presumed common mechanisms. At other times, it has moved toward increasingly fine-grained distinctions, carving syndromes into narrower subtypes in the hope of diagnostic precision, prognostic clarity, and targeted treatment. Each swing has been accompanied by a sense that the current framework finally “gets it right,” only to be followed by revision as anomalies accumulate.
Large-scale genetic findings like these offer a compelling biological explanation for why neither extreme has ever fully succeeded. If multiple psychiatric syndromes share substantial genetic architecture, then comorbidity is not an artifact of poor interviewing or diagnostic sloppiness, but an expected consequence of overlapping vulnerability systems expressing themselves differently across development, context, and stress. The apparent neatness of our diagnostic manuals may therefore obscure a far messier underlying reality.
Importantly, this does not invalidate diagnosis itself, nor does it imply that all conditions should be collapsed into a single undifferentiated category. Lumping and splitting are not opposing dogmas so much as complementary lenses. Lumping has value when the goal is to understand shared mechanisms, reduce artificial boundaries, recognize common trajectories, and avoid reifying distinctions that lack biological or clinical robustness. Splitting, by contrast, becomes indispensable when precise phenomenology matters—when predicting course, tailoring treatment, communicating risk, or conducting focused research on well-defined clinical problems.
In practice, good psychiatry has always involved knowing when to do each. A clinician may need to lump in order to see the larger pattern of vulnerability, suffering, and adaptation in a patient’s life, while simultaneously splitting enough to recognize specific syndromes that carry distinct risks or treatment implications. The emerging genetic evidence does not demand allegiance to one approach over the other; rather, it reinforces the wisdom of holding our categories lightly, using them pragmatically, and remaining open to revision as our understanding deepens.
Seen this way, the enduring oscillation between lumping and splitting is not a failure of the field, but a reflection of the complexity of the phenomena it seeks to describe.

